US Navy working on 'smart' prosthetics for amputee war veterans
The prosthetics would use a range of sensors to monitor the walking gait of the patient as well as potential infection risks.
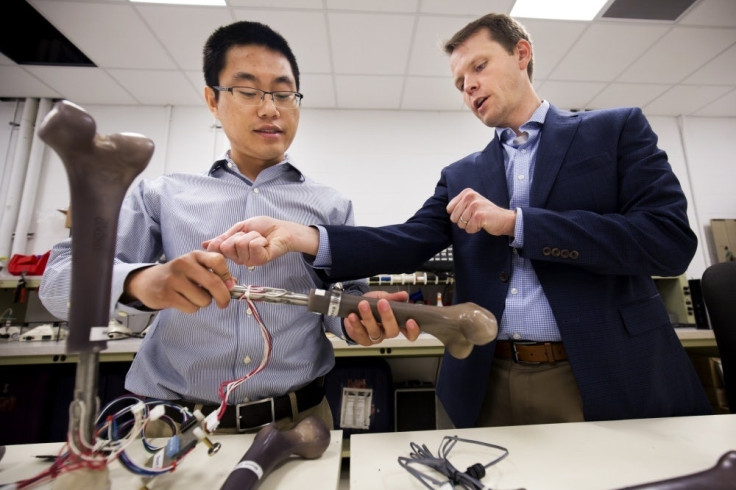
The US Navy is working on a special form of prosthesis – a smart artificial leg that could be attached and detached at will as well as monitored to keep an eye on the walking gait and potential infection risks.
Scientists from the Office of Naval Research (ONR) have partnered with Walter Reed National Military Medical Center, the Naval Research Laboratory and a number of universities to develop the new smart artificial limb for warfighters, who suffer from the partial loss of or one or both of their legs.
The limb, which is a part of the broader Monitoring OsseoIntegrated Prosthesis (MOIP) project, could usher the next-generation of prosthetics, giving amputees a number of benefits over conventional prosthetics that fit residual limb with a socket while exerting pressure on the limb's soft tissue and causing severe pain, sores, blisters, and infections.
The whole thing will work with the help of a titanium fixture that is surgically implanted into the thigh bone, which grows around the point of insertion, leaving only a small connector protruding from the remaining leg. This connector could then be used to attach or detach the artificial limb at will.
As there's no pressure on the soft tissue in the case, the limb could prove extremely comfortable for the wearer and allow for a more natural walking motion. Plus, it will also incorporate a range of sensors which evaluate the prosthetic's strength, body stress placed on it, and any changes to wearer's movement or walking gait over time.
But, it is important to note the problem of infection won't get solved with the smart limb or its sensors (metal sticks out of the residual limb and could still prove infectious). For this, a critical bio-compatible sensor array will be embedded into the amputee's residual limb.
Once embedded, it would constantly monitor indicators of infection such as changes in body temperature and pH balance and track how well the bone is fusing with the prosthetic. This could help doctors treat or prevent the spread of the infection at the first place.
Professor Jerome Lynch, who is overseeing the sensor array's development, says, "One game-changing application of this technology would be as a tool to inform doctors when prostheses can be safely loaded after surgery, leading to more accurate determination of when patients are ready for physical therapy after receiving a new prosthetic".
© Copyright IBTimes 2024. All rights reserved.





