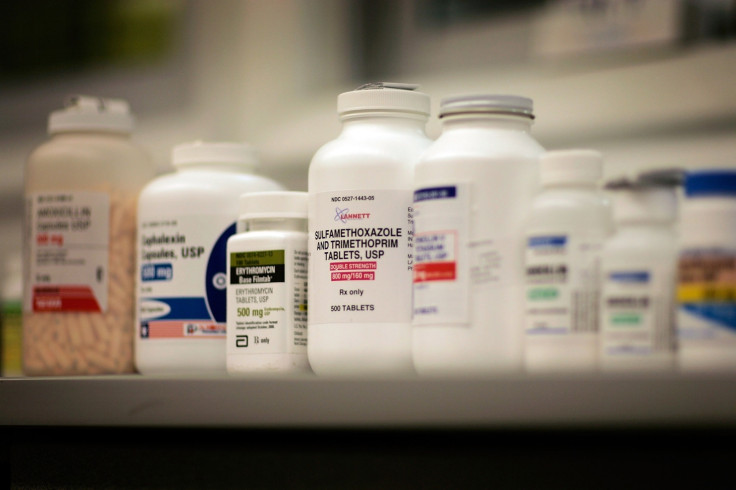
Why you shouldn't take antibiotics if you have a cold
If patients don't stop demanding antibiotics, experts fear that infections will kill more people than cancer by 2050.
Patients are being urged to stay at home and rest when suffering from common illnesses rather than demanding antibiotics from their doctors, in an attempt to avoid what has been widely described as the antibiotic apocalypse.
Public Health England (PHE) has revealed that a fifth of prescriptions for antibiotics are being given to patients who do not need them, as doctors bow to pressure to hand out medication - even if it has no health benefits.
In fact, using antibiotics when they are not needed can harm a person's health by attacking so-called friendly bacteria, and prompts the microbes to mutate and survive antibiotic treatment, seen most recently in the rise of super-gonorrhoea.
The issue of antimicrobial resistance on a public health level has become such a pressing concern that the United Nations this year formed an interagency group to swerve a global post-antibiotic era, when routine procedures including cesareans as well as cancer treatment could become too risky to perform.
Meanwhile in the UK, the government is rolling out an awareness campaign with the jingle: "Antibiotics, we're wonderful pills/ but don't ever think we'll cure all of your ills. Take us for the wrong thing that's dangerous to do/ when you really need us we could stop working for you."
The reason that antibiotics can be used to treat some conditions and not others is that these drugs only target bacterial infections, whereas most common colds are caused by viruses.
Bacteria are relatively complex single-celled organisms which can reproduce on their own. Fewer than 1% of bacteria cause diseases, while the rest aid the body in digesting food, fighting other microbes and cancer cells as well as providing nutrients. Severe infections such as pneumonia, sepsis, bacterial meningitis, tuberculosis, salmonella and whooping cough are caused by bacteria and fought with antibiotics.
Viruses, however, are smaller than bacteria and made up of genetic material known as DNA or RNA, and almost always cause disease. In order to survive and reproduce, they must hijack and reprogram a host cell.
Most viruses die when the microbe they latch onto bursts and dies, but some will transform cells into malignant or cancerous cells.
Bacteria can, therefore, be killed using antibiotics, while the least severe viruses, such as the common cold and flu, generally die of their own accord. Viruses can be prevented and treated with vaccines and drugs - just not antibiotics.
But as both common viruses and bacteria can trigger similar symptoms - from a runny nose to a sore throat - and spread similarly, it is easy to confuse the two.
Since the government first launched its five-year antimicrobial resistance strategy in 2013, GPs have issued around 2.5 million fewer antibiotic prescriptions - dropping by 13% from the peak in 2014.
Still, drug-resistant infections killed an estimated 5,000 people in England each year, while four in 10 cases of bloodstream E. coli are no longer treatable with first-choice antibiotics, according to PHE. If patients don't stop demanding antibiotics, experts fear that infections will kill more people than cancer by 2050.






