Scientists create new skin patch in breakthrough which makes wounds heal faster and reduces scarring
The key ingredient is a protein which can be harvested directly from a patient undergoing surgery and turned into an instant healing agent.
A new skin patch has been developed which could help wounds heal faster while minimising the formation of scars.
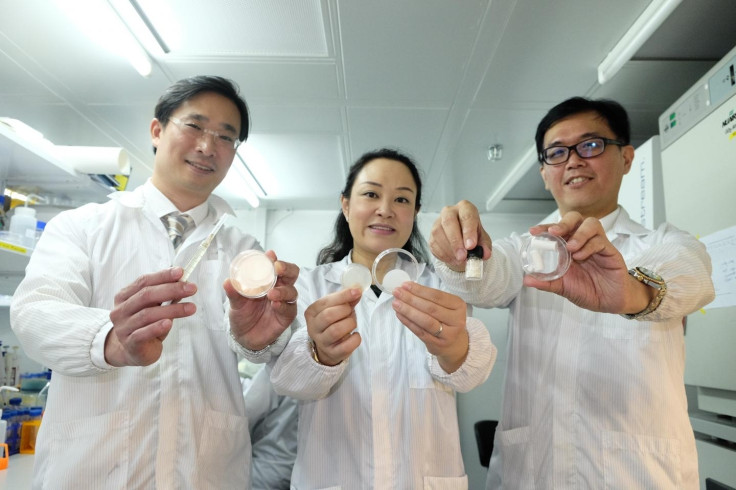
The gel patch created by scientists from Nanyang Technological University, Singapore (NTU Singapore) is currently at the prototype stage. But once it is fully developed, it could be hugely beneficial to everyone from patients undergoing surgery, diabetics who have hard-to-heal skin lesions and others with skin wounds.
Similar patches which either reduce scarring or improve healing have been developed before. However, the new prototype is the first to do both simultaneously.
The research detailing the skin patch is published in the journal Scientific Reports.
In the study, the team found that a protein – called Angiopoietin-like 4 (ANGPTL4) – reduced inflammation in the early phase of wound healing in mice and subsequently helped the formation of new blood cells and cell growth, while also reducing scarring.
Scars occur when too much collagen – the most abundant protein in our bodies – assembles in one place.
"To reduce scars, all we had to do was to find a 'tuning knob' that controls the amount of collagen produced, instead of turning it off completely which is what typical anti-scarring medicine does, and which could interfere with the healing process," said Andrew Tan, co-leader of the study from NTU's School of Biological Sciences.
After the application of ANGPTL4, the mice wounds healed more effectively and three times faster than normal. In light of this, the researchers developed a patch which was enriched with the protein.
Intriguingly, the team say that the active ingredient in ANGPTL4 can be harvested directly from discarded fatty tissues taken from patients in hospitals.
"The easy extraction of ANGPTL4 also could mean that in future, a surgeon can use the patient's fat and turn it into a healing agent on the spot, to promote faster recovery of the patient's wounds after an operation," said Cleo Choong, the other co-leader of the study from NTU's School of Materials Science and Engineering.
"In addition, we have developed ways to package ANGPTL4 into easy-to-use formulations such as gel patches, topical creams and injectable microcapsules. This will make it easy for doctors and even patients to use in future, should the product be made available to the market," she said.
Typical anti-scarring treatments target a kind of "on-off switch" for collagen production. When this biological 'switch' is turned off, collagen production stops and there is no scarring. However, collagen is needed in various processes related to the repair and regeneration of damaged skin, so stopping its production could be counterproductive.
So, to work out a way to control the amount of collagen produced and where it assembled, the team investigated what exactly causes production of the protein to go into overdrive when a wound occurs.
They found that another protein called Scleraxis was working with the biological collagen "off-switch" whenever scars are produced. Furthermore, they showed that ANGPTL4 actually interferes with Scleraxis, resulting in reduced scar collagen production.
The team hope to refine their prototype before conducing further lab experiments and clinical trials.
© Copyright IBTimes 2025. All rights reserved.





















