Skin transplants from dead people can heal wounds faster
Scientists from the University of Manchester have discovered that the skin of dead people that has had its cells removed can help chronic skin wounds on the living to heal much faster.
This new technique of using real human skin is a departure from the skin substitutes that have been developed by scientists over the years to treat wounds.
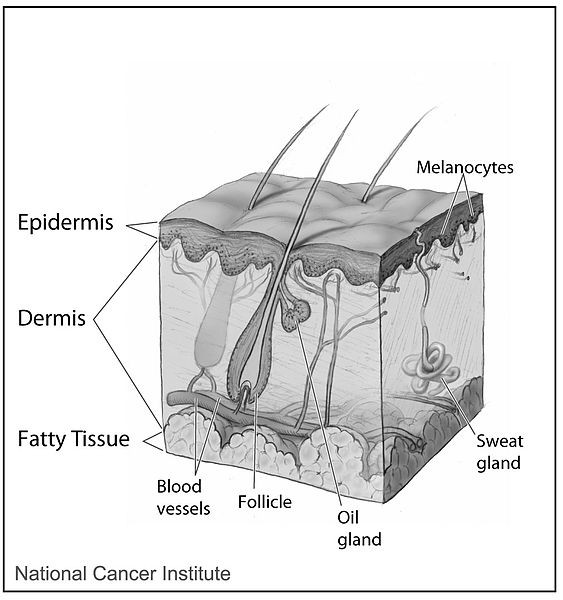
Skin substitutes, which are becoming more effective, help to treat wounds by aiming to mimic the body's extracellular matrix, i.e. the complex scaffolding of proteins and other compounds that help bind cells together.
Removing cells from human skin
The researchers took skin from human cadavers and first used antibiotics to decontaminate the skin, before removing all the cells from the skin using a combination of enzymes, detergents and other chemicals.
"The skin is the largest organ in the human body, and the skin we work with is just like any other organ donated by people," Ardeshir Bayat, a bioengineer and clinician-scientist at the University of Manchester who is senior author of the study, told Live Science.
This "decellularised" skin is effective in helping to heal acute skin wounds, such as burns, painful ulcers, severe injuries and chronic skin wounds, which can take between six and eight weeks to several years to heal.
"Imagine a house with all the furniture and people taken out — you're left with an empty shell that is easier to populate than just building a house from scratch," said Bayat.
"In the same way, decellularised dermis provides a scaffold that the body can try to populate with its own cells. The good thing about decellularised dermis is that it has a structure and composition that the human body is already used to — the body responds more favourably to what it is used to than what it isn't."
By removing all the cells, the decellularised skin no longer triggers immune reactions, so the recipient's body won't reject it.
Best at triggering blood vessel growth
The researchers removed four disks of skin measuring 5mm wide (0.2 inches) each from 50 healthy volunteers.
Of the four disks taken from each volunteer, the first wound site was left alone, the second wound site had the removed skin re-inserted, another wound site was treated with an artificial skin substitute and the final wound site was treated with the decellularised skin.
The researchers discovered that out of the four, decellularised skin was the best at triggering growth of new blood vessels, and the skin tissue that grew from this type of skin was also comparable in strength and other properties to normal skin.
"We had a patient, a 92-year-old lady, who had a skin ulcer for 20 years, even after getting treated with various dressings," Bayat said. "After we treated her with decellularised dermis, she healed within four weeks."
The results of the study are detailed in a paper entitled Acute Cutaneous Wounds Treated with Human Decellularised Dermis Show Enhanced Angiogenesis during Healing in the journal PLOS ONE.
© Copyright IBTimes 2025. All rights reserved.






















