China's gene-editing experiments open the door to a world of ethical dilemmas
Science is advancing rapidly, so we need to address the long-term implications of altering our genetic makeup.
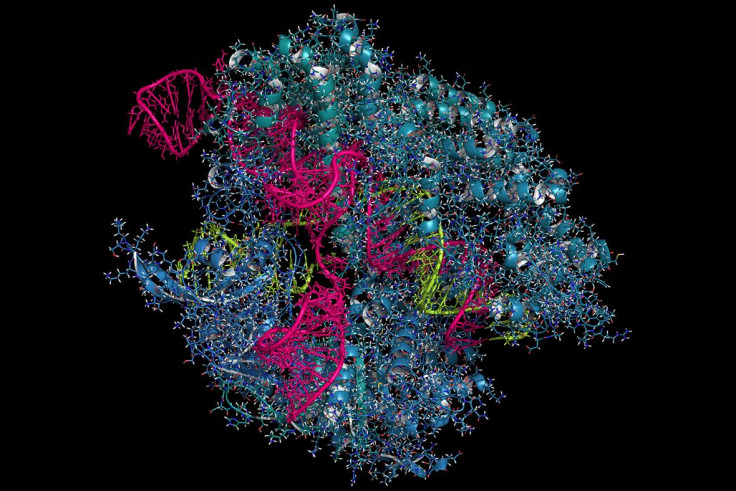
Chinese scientists at Sichuan University have pioneered another first in biotechnology: injecting lung cancer patients with genetically modified cells using the cutting-edge CRISPR technique – one that is behind a flurry of recent innovations. And in the US, scientists at UC San Diego also recently demonstrated that blindness in adult mice could be partially reversed using an elaboration on CRISPR.
The speed of these recent developments has alarmed some, underscoring worries that our science is advancing faster than our ability to fully appreciate the ethical and social ramifications of genetic engineering. The Sichuan and San Diego trials, in and of themselves, do not appear particularly problematic, but they do raise questions about the long-term implications of perfecting the ability to alter our genetic makeup. These are questions that societies will need to begin debating in earnest now, as the science is indeed advancing extraordinarily rapidly.
Old, but new
Gene therapies have been in use for decades, but the CRISPR technique has proven to be a more accurate and effective means of targeting specific troublesome genes to be knocked out. The Sichuan trial involves taking a patient's own immune cells, modifying them using CRISPR, then re-implanting them in the patient, in the hopes that the modified cells will effectively combat the patients' cancer.
This is what is known as a Phase I clinical trial, and is mostly trying to determine whether the intervention is safe or has serious side effects. The sample size of 10 participants is too small to prove that the technique is effective in treating cancer, but can reveal whether there are significant safety concerns. If all goes well, further trials with more subjects would be conducted to demonstrate effectiveness.
As a first-in-human trial, the risks are inherently uncertain and side effects could be significant. But this is true of many novel interventions. Sichuan University's research ethics committee will have had to assess the potential risks and benefits, and evidently concluded that the ratio was acceptable (along with a plethora of other ethical requirements, like consent and continuing review).
The trial is being run in patients for whom conventional therapies have failed, so that even a small chance of benefit may be worthwhile. And even if the trial fails due to significant adverse events, the knowledge generated will help contribute to the development of safer and effective interventions in the future.
Ethical dilemmas
It is important to note that the Sichuan and San Diego trials involve somatic gene editing – editing genes of adult cells that will not be passed on to subjects' offspring. This is much less controversial than germline gene editing, where changes to genes in gametes or embryos can be passed on to future generations. An earlier Chinese trial at Sun Yat-Sen University caused significant controversy because it involved modifying human embryos using CRISPR – germline changes that could be passed on to future generations. The embryos were destroyed after the trial, and so would never be brought to term, but the idea of altering the human germline was evidently disturbing to many.
Without international alignment more cases of rogue scientists seeking out unregulated contexts to perform questionable genetic modification therapies will undoubtedly emerge
In 2015, a summit of US, UK and Chinese national academies convened to discuss these controversies and released a consensus statement: somatic gene therapies are not particularly objectionable, as long as the benefits are proven to outweigh the risks. But the summit concluded that germline therapies are too problematic to pursue in humans presently. (Notably, the summit was accepting of pre-clinical experiments on germline modification, such as the Sun Yat-Sen University experiment where no modified humans were born).
The worries over germline modifications include scientific and safety concerns - that the technology is too new, unproven and risky to begin human trials. But deeper ethical and social concerns have also arisen that merit wider discussion. Germline modification is arguably more far-reaching than somatic, raising the question of whether it is fundamentally altering human nature – and whether doing so to prevent disease is to be avoided, or embraced.
Furthermore, they raise the spectre of genetic enhancement: using gene-editing techniques to improve capacities like intelligence, athletic abilities, or lifespan. And again we must ask, is that a good or bad thing? Will its social disruptions improve the prospects of humanity, or exacerbate inequalities and bring us one step closer to a Brave New World?

Continuing a conversation
Even though the Sichuan and San Diego trials are somatic and quite limited, they are part of a broader rapid advancement of genetic engineering. Improvements in somatic therapies will likely also make germline modification more efficient and easier to perform. For this reason, it is important for societies across the globe to seriously consider the ethical and social implications of these gene-editing technologies, to debate the kind of world we want to live in, and align research agendas and regulatory regimes to realise those goals.
Arguably, the first baby with germline genetic modifications has already been born, using an entirely different technique of mitochondrial replacement therapy. In order to avoid passing on a mitochondrial disorder, a couple underwent in vitro fertilisation to create an embryo, but then had the embryo's mitochondrial DNA (making up a small but important portion of one's overall genetic makeup) hollowed out and replaced with a third individual's mitochondrial DNA. This can be considered a germline modification, as the baby's mitochondria will be passed on to their children.
Notably, the couple were American but the operation had to be performed in Mexico due to US restrictions. This just highlights how rapid advancements in genetic modification will enable a wide variety of agents to engage in ethically controversial activities. The UK has taken the lead in careful oversight and regulation of mitochondrial replacement therapy, but without international alignment more cases of rogue scientists seeking out unregulated contexts to perform questionable genetic modification therapies will undoubtedly emerge.
A sustained international debate over genetic modification is therefore needed, both to explore the tough ethical, social and scientific questions raised, and to move towards international harmonisation. Even if completely consistent regulations are out of reach, broad consensus and soft pressure to conform to international norms will go a long way towards ensuring responsible, responsive genetic modification in the years to come.
Dr G. Owen Schaefer is a Research Fellow in Biomedical Ethics at the National University of Singapore
© Copyright IBTimes 2025. All rights reserved.