HIV holy grail: Scientists train immune system to spot and destroy hiding mutated virus
Scientists from Johns Hopkins University School of Medicine, University of California, San Francisco and Yale University have made a breakthrough in the fight to eradicate HIV, by figuring out how to train immune cells to locate and destroy mutated forms of the virus.
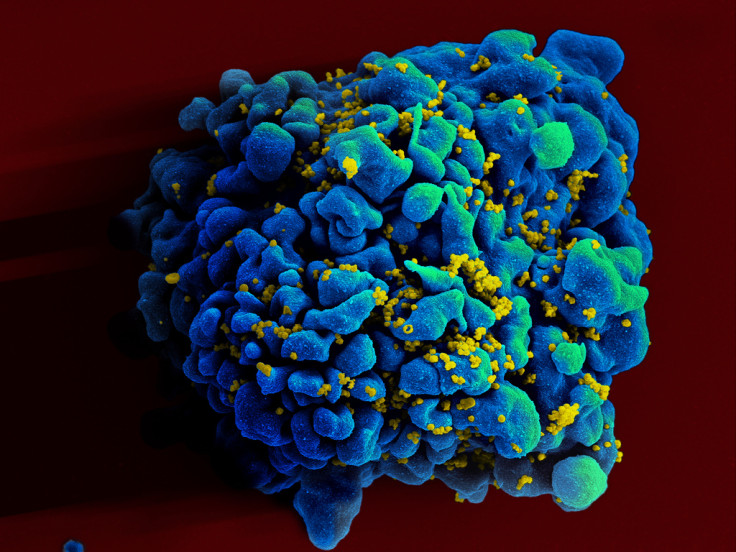
The biggest problem today in HIV treatment is once a patient is infected with the virus, it hijacks a class of immune cells known as memory CD4+ T cells.
The virus shapeshifts and hides in these infected, mutated cells, which causes the immune system no longer recognise it to be a threat, and so far, attempts to lure HIV out of its dormancy and kill it have failed.
Their research, entitled "Broad CTL response is required to clear latent HIV-1 due to dominance of escape mutations" is published in the journal Nature.
"Our results suggest that luring HIV out of hiding is winning only half the battle," said senior investigator Robert Siliciano, MD, a professor of medicine, molecular biology and genetics at the Johns Hopkins University School of Medicine, who was a lead investigator of the study.
"We found that these pools of dormant virus carry mutations that render HIV invisible to the very immune cells capable of disarming it, so even when the virus comes out of hiding, it continues to evade immune detection."
Antiviral drugs prevent HIV from mutating
The researchers deployed a technique called deep sequencing, which reveals HIV's genetic features down to a single infected cell.
Using deep sequencing, they analysed blood samples from 25 patients infected with HIV – 10 of whom had started therapy within three months of the infection, while the rest began treatment after the HIV infection entered its chronic stage.
All viruses and bacteria carry key protein identifiers. When these are kept intact, the immune system is able to recognise these cells are foreign to the body and then seeks to destroy them.
The researchers discovered that in patients who had begun antiviral therapy within a few weeks or months of being infected, the HIV cells' protein identifiers were largely unaltered as the treatment had managed to halt the virus' mutation process and freeze it in its original state.
However, in patients who had started treatment later on, the key protein identifiers had been mutated by the HIV to make them unrecognisable to the immune system.
Mixing T cells with mutant HIV
The researchers isolated killer T cells from the patients and mixed them either with mutant forms of HIV or with a cocktail that contained both mutated and non-mutated lab-made chunks of HIV protein.
When these new souped-up T cells came into contact with HIV cells taken from patients that contained escape mutations, the T cells killed 61% of the HIV cells in the laboratory petri dish.
And when the T cells were injected into mice infected with mutated HIV cells, the souped-up T cells were able to control the infection and cause a thousand-fold drop in the amount of virus circulating around the body, and some of the mice had HIV that was suppressed below detectable levels.
"We hypothesised that if these killer T cells were somehow nudged to spot the tiny segments of unaltered virus, they would kill the entire HIV-infected cell," said Kai Deng, lead author of the study and a postdoctoral research fellow at the Johns Hopkins University School of Medicine.
"Our results shows that any curative strategy designed to eradicate HIV infection would need to include the use of killer T cells primed to recognise non-mutant forms of HIV."
© Copyright IBTimes 2025. All rights reserved.




















