'Virtual heart' predicts risk of sudden cardiac death from arrhythmia
A 'virtual heart' that is four times better at predicting sudden cardiac death than the current method has been created by scientists. A proof of concept study suggests this virtual heart could be used to help doctors pinpoint patients who need treatment for cardiac arrhythmia.
Arrhythmia is a condition where the heart's rhythm is either too fast, or too slow. Heart attack survivors are at risk of the condition as the attack can leave behind damaged cardiac tissue. Arrhythmia can also lead to fainting, chest pain, stroke, and even sudden death.
Currently, physicians look at how much blood is being pumped out of the heart to assess the risk of onset arrhythmia. If there is a risk of arrhythmia, they will recommend implantable defibrillators to control the heart's electrical signals.
However, researchers from Johns Hopkins University say this method of assessing arrhythmia risk is imprecise. Those who do receive the implant may not see any beneficial result from it, but assume all the risk of an invasive heart operation.
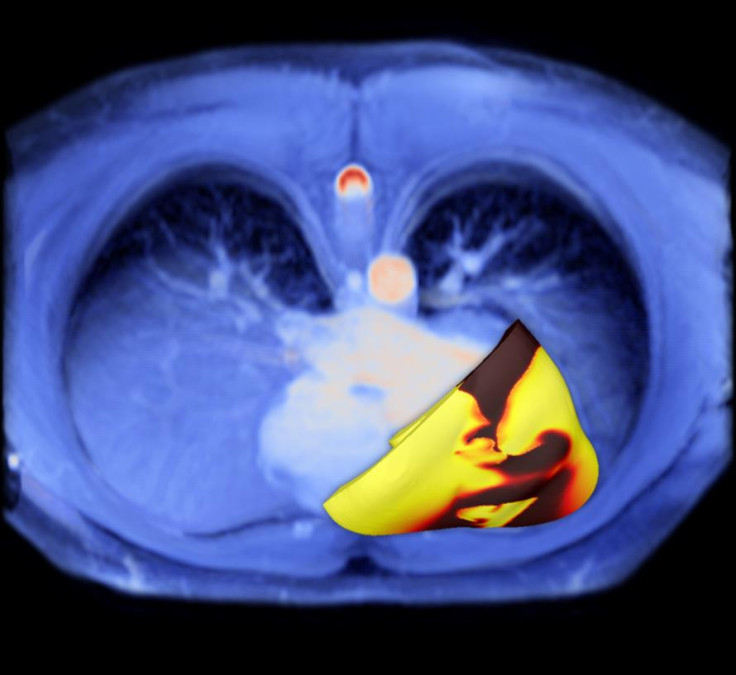
To make tests more precise, the scientists developed a computer-generated 3-D virtual heart. It uses Magnetic Resonance Imaging (MRI) scans to generate a personalised model of the patient's heart. The researchers can then use the model to assess their risk of developing arrhythmia by running simulations on it.
The scientists used 41 heart attack survivors to test their risk of developing arrhythmia. They analysed their risk using their virtual heart, and the currently used blood pumping method. All patients had received implants because their test scores indicated they were at risk of arrhythmia. Researchers then compared both methods of prediction, looking at which patients went on to develop arrhythmia.
Results, published in the journal Nature Communications, showed patients who tested positive for arrhythmia through the artificial heart were four times more likely to develop the condition in real life than those who tested negative. The artificial heart was also shown to be four to five times better than existing methods at predicting arrhythmia.
"We demonstrated that [the virtual heart] is better than any other arrhythmia prediction method that is out there," said Natalia Trayanova, a researcher working on the study. "By accurately predicting which patients are at risk of sudden cardiac death, the [virtual heart] approach will provide the doctors with a tool to identify those patients who truly need the costly implantable device, and those for whom the device would not provide any life-saving benefits."
The researchers hope to continue testing their virtual heart model. Further tests on a larger group of patients will provide the scientists with more accurate data. Katherine Wu, a cardiologist working on the study, said: "This is a ground-breaking proof-of-concept study for several reasons. We were able to test the heart virtually to see how irritable it is under certain situations. We could do all this without requiring the patient to undergo an invasive procedure. This represents a safer, more comprehensive and individualised approach to sudden cardiac death risk assessment."
© Copyright IBTimes 2025. All rights reserved.




















