Antibiotic-resistant superbugs can defeat drugs we haven't even invented yet
MRSA was resistant to methicillin 14 years before the drug was first used.
Normally it's thought that resistance to antibiotics only evolves when we start using those drugs against bacteria. So how can resistance to the antibiotic methicillin have existed more than a decade before it was first used?
Antibiotic resistance is a growing problem. In Europe alone it kills hundreds of people a week, with infections resistant to all available antibiotics on the rise.
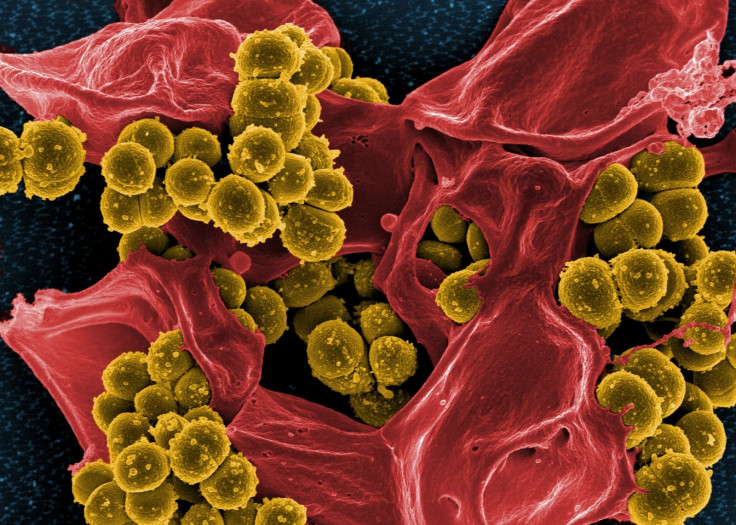
A study has now found that methicillin-resistant Staph aureus (MRSA) existed in the mid-1940s – a full 14 years before the drug was first used in 1959. The discovery suggests that in the arms race against antibiotic-resistant bacteria, the superbugs are one step ahead.
The finding comes from analysis of 209 historic samples of Staph aureus, deposited in archives in the UK, Denmark and the US. The samples were collected from hospital patients and cases in the community, sent to clinical laboratories and from there to reference labs.
They were kept because they had an unusual resistance pattern, showing resistance to penicillin, streptomycin and tetracycline – all very common antibiotics for the time.
"These institutions stored these isolates over decades, so we had the opportunity to go back and resurrect and sequence them, in a way not possible when they were first collected," study author Catriona Harkins of the University of Dundee told IBTimes UK.
The gene mecA gives Staph aureus resistance to methicillin by producing a protein called PBP2a. This makes antibiotics less efficient in binding to the bacteria's cell wall. The first bacteria to have this gene were around as early as the mid-1940s. But the first observation of methicillin-resistant Staph infections were in 1961.
So how did the bacteria end up with resistance to a weapon against them that hadn't been invented yet?
"In most instances we consider the development of resistance is an adaptation to combat something we're using to try to eradicate it," said Harkins.

"But what we actually think happened was that when Staph aureus was treated widely in the 1940s with penicillin, this element [mecA] was acquired by the organism and it gave it an additional mechanism to resist penicillin. And it also gave the bacterium resistance to methicillin when it was introduced."
It might seem unusual for the defence to come before the weapon, but, given the amazing adaptability of bacteria, perhaps we shouldn't be surprised.
"Staph aureus is able to survive in so many different environments and has so many different hosts. Every time we've introduced an antibiotic, Staph aureus has developed a way to resist it. Microorganisms are so readily able to adapt that now we just watch for this coming."
But the findings of this study also bring hope for new ways to tackle superbugs – if not in new antibiotics, then in the importance of tracking when and where resistance evolves to be able to preempt it.
"It's kind of a cautionary tale from a long time ago. If we introduce something new or change our practice, we have to survey what's happening to microorganisms – forewarned is forearmed."
© Copyright IBTimes 2025. All rights reserved.






















