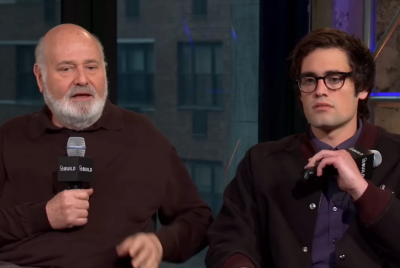
Inside Schizophrenia: Symptoms, Causes and Treatment After Shocking Rob Reiner Family Tragedy
The high-profile case has renewed scrutiny of severe mental illness

The alleged killing of Hollywood filmmaker Rob Reiner and his wife, Michele Singer Reiner, by their own son has sent shockwaves through the entertainment world and ignited renewed scrutiny of severe mental illness and substance abuse.
According to reports, the couple's son, Nick, who has been charged in connection with their deaths, was suffering not only from substance abuse issues but also from schizophrenia, a serious psychiatric disorder that experts say can become dangerously destabilising if untreated or poorly managed. The devastating case has thrust the intersection of mental illness, addiction and family safety into the global spotlight.
What Happened in the Case of Rob Reiner's Son
While the criminal proceedings are still in their early stages and the allegations have yet to be tested in court, the circumstances surrounding the deaths have sparked intense public debate about medication adherence, long-term psychiatric care and the warning signs that may be missed even within families.
Mental health professionals caution that schizophrenia remains widely misunderstood and heavily stigmatised, particularly when it becomes associated with violent crime. They stress that most people living with the condition are not violent, but that co-occurring substance abuse can significantly worsen symptoms and impair judgement.
Authorities have confirmed that the investigation remains ongoing, with further court hearings expected. Prosecutors have emphasised that no conclusions should be drawn ahead of trial, while defence representatives have not publicly outlined their legal strategy.
As the case continues to unfold, it has cast a harsh light on the fragile balance between mental health treatment, addiction support and public safety — raising questions that experts say are often only confronted after irreversible tragedy.
Why Schizophrenia Is Central to the Case
Schizophrenia has become central to public discussion following reports that the accused had a documented history of mental illness. Specialists caution that this context should not be interpreted as evidence that schizophrenia causes violent behaviour.
Studies consistently show that most people living with schizophrenia are not violent and are more likely to be harmed than to harm others. However, untreated symptoms, medication disruptions and co-existing substance use can significantly worsen outcomes.
What Schizophrenia Is
Schizophrenia is a chronic psychiatric disorder that affects perception, thinking and emotional regulation. It typically develops in late adolescence or early adulthood and affects around 1% of the global population, as reported by the National Library of Medicine. Diagnosis is based on clinical assessment over time rather than a single medical test.
The condition varies widely in severity, with some individuals experiencing episodic symptoms while others require long-term support.
Schizophrenia Symptoms and Early Warning Signs
Symptoms are broadly categorised into positive, negative and cognitive types. According to the National Health Service, positive symptoms include hallucinations, delusions and disorganised speech. Negative symptoms involve social withdrawal, reduced emotional expression and loss of motivation. Cognitive symptoms affect memory, attention and decision-making.
Clinicians warn that escalating symptoms can impair judgement and daily functioning, particularly if treatment is interrupted.
Schizophrenia Cause: What Science Currently Knows
There is no single cause of schizophrenia. WebMD research points to an interaction between genetic risk, brain chemistry differences and environmental factors such as early trauma or drug exposure. Recent genetic studies suggest schizophrenia shares biological pathways with other psychiatric disorders, helping explain overlapping symptoms.
Schizophrenia Treatment and Ongoing Challenges
Treatment commonly involves antipsychotic medication alongside psychological therapy and community-based support. While medication can be effective in reducing hallucinations and delusions, side effects and changes in treatment can complicate care.
Mental health advocates say the case underscores the importance of sustained access to psychiatric services, close monitoring and early intervention to prevent crises.
© Copyright IBTimes 2025. All rights reserved.