Easier and cheaper way to detect cancer cells using sound waves developed
Researchers have demonstrated the detection of cancer cells in blood using an inexpensive and efficient method that could replace invasive biopsies.
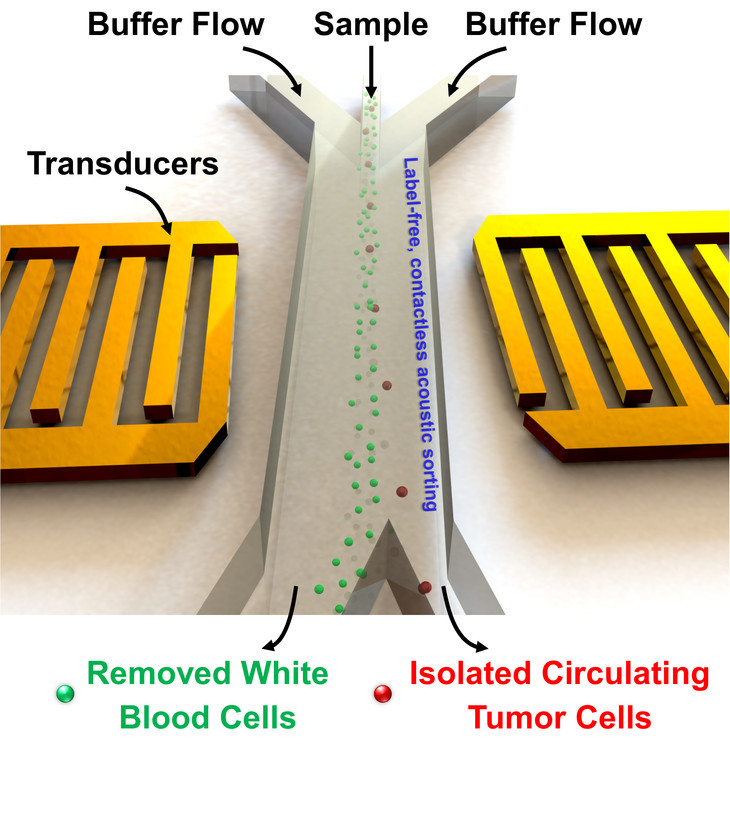
The method called acoustic tweezers makes use of sound waves and a disposable chip to separate cancer cells from blood cells.
Cancer cells often break free from their original locations and circulate through the bloodstream, but finding them can be challenging as there may be just one such cell in every one billion blood cells.
Existing methods require large quantities of appropriate antibodies that bind to cancer cells and help isolate them. For this the antibodies have to be known.
Other methods are complex requiring high speed centrifuges to separate the cells and can damage the cells.
The sound waves, on the other hand, do the job at much lower costs and very quickly. It takes about five hours for the tiny device to separate cancer cells from a typical patient sample of about six millilitres.
The team from Pennsylvania State University, MIT and Carnegie Mellon tested the device with blood samples from three breast cancer patients and found the method to be as effective as a commercially available device.
Acoustic-based separations are non-invasive and do not alter or damage cells. The new device improved cell sorting throughput more than 20 times higher than previously achieved.
The surface acoustic waves can separate cells using very small amounts of energy. They are safe too as the power intensity and frequency are similar to those used in ultrasonic imaging, safe even for foetuses.
"In order to significantly increase the throughput for capturing those rare CTCs, device design has to be optimized for much higher flow rates and longer acoustic working length," said Ming Dao, principal research scientist, materials science and engineering, Massachusetts Institute of Technology.
The findings are published in the US journal Proceedings of the National Academy of Sciences.
The method works on the principle of how two sound waves of the same wavelength travelling from opposite directions will cancel each other at a point.
Sound waves can push very small objects like a cell to that point from where they are collected into the fluid stream that moves the separated cells along.
Technique used
The researchers made use of differential size and weight of the different cells to choose appropriate acoustic pressures that pushed the CTCs out of the fluid stream and into a separate channel for collection.
Each cell experiences the acoustic wave for only a fraction of a second. In addition, cells do not require labelling or surface modification.
As the sound waves are tilted, they run across the micro-channel at an angle causing each cell to encounter several pressure nodes in the channel.
The cells are pushed further to the side of the channel and the distance they move depends on their size and other properties.
The researchers saw a separation rate of more than 83% when they used two types of human cancer cells, similar in size -- HELA cells and MCF7 cells; so also on other cancer cells.
Once optimised, physicians can use the devices to monitor how patients react to chemotherapy, for initial diagnosis and for determining treatment and prognosis.
"This work, involving a highly cross-disciplinary group of medical doctors, engineers, computational biologists, and device experts, has led to the design and development of a label-free platform for identifying and separating CTCs while preserving the integrity of the cell," said Subra Suresh, president, Carnegie Mellon University and co-author of the work.
"It promises to offer new avenues for basic research into the pathology and metastasis, and for clinical diagnosis of rare tumour cells."
© Copyright IBTimes 2025. All rights reserved.





















