Completing full course of antibiotics may 'do more harm than good'
There's never been any solid evidence that finishing the course of antibiotics is beneficial.
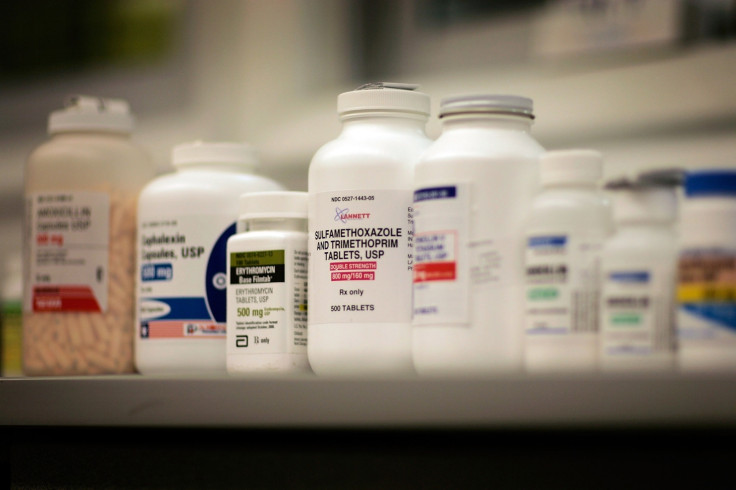
Everything you know about taking the full course of antibiotics might be wrong. Doctors are now saying that completing the full course of antibiotics might in fact increase your chance of creating antibiotic-resistant bacteria.
It's a familiar warning to anyone who's been prescribed antibiotics: it's vitally important that you take the full course, and don't stop even if you start to feel better. But now doctors are saying that that advice has no basis in evidence.
In fact, the reverse might actually be true, and taking an unnecessarily long course of antibiotics could boost the chances of developing and spreading drug-resistant infections. The latest call for a change in advice to patients is published in an article in the BMJ.
Taking a full course of antibiotics after the symptoms of the illness have passed exposes many kinds of bacteria in the body – not just the ones causing the illness – to antibiotics.
Many of the bacteria that are prone to causing dangerous antibiotic-resistant infections, such as Staph aureus and E coli, live on the body harmlessly without causing a problem most of the time. If these bacteria are exposed to excess antibiotics, there is more chance that they could start to develop resistance.
So in other words, shortening a course of antibiotics to the bare minimum to fight the illness might be the best way to minimise the risk of resistance. This is a large and growing problem – the equivalent of a full Boeing 747 die from antibiotic-resistant infections each week in Europe alone.
How did the idea of 'completing the course' come about?
"We didn't understand the advice and wanted to know where it came from, and on what bases it was given," article author Tim Peto of the Oxford Biomedical Research Centre told IBTimes UK.
"We did find a reference to this idea by Alexander Fleming, who discovered penicillin and got the Nobel Prize for it."
In his speech accepting the prize on 11 December 1945, Fleming outlined the dangers of not using enough penicillin to treat an infection. "If you use penicillin, use enough," Fleming warned. But no one has seriously thought to question this wisdom since.
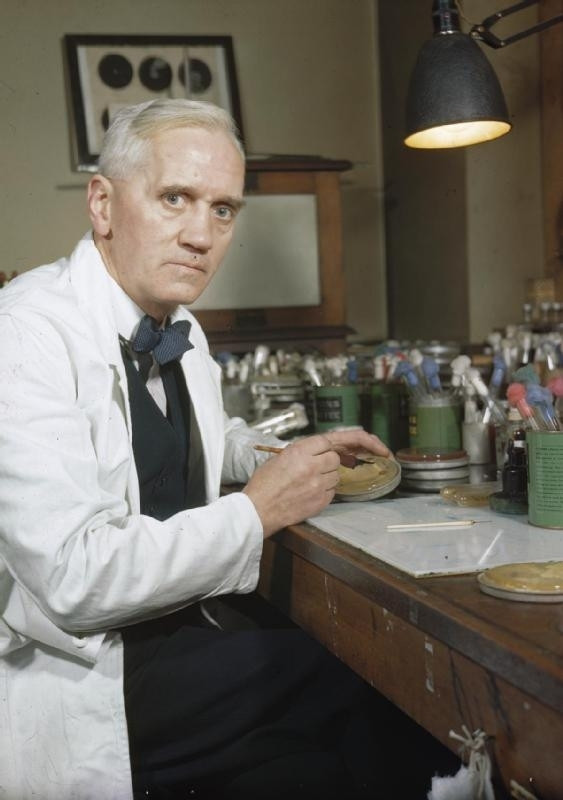
"We suspect that no one wanted to challenge a Nobel laureate. So it got embedded in peoples' belief systems. We want to highlight that it wasn't evidence based," Peto said.
"The public health messages on antibiotics are confusing. That's because we haven't got enough high-quality, solid research to inform policy. And so there's a slight information vaccuum."
Time for change?
Other researchers have welcomed the study. Jodi Lindsay, professor of microbial pathogenesis at St George's, University of London, said that stopping the course of antibiotics when you feel better is a sensible message to take from this paper.
"The evidence for 'completing the course' is poor, and the length of the course of antibiotics has been estimated based on a fear of under-treating rather than any studies," Lindsay said.
"The evidence that using less overall antibiotics will reduce antibiotic resistant infections is solid. Therefore, the overall message to conserve precious antibiotics is simple and important."
Mark Woolhouse, professor of infectious disease epidemiology at the University of Edinburgh, agreed that doctors' advice to patients needs to change.
"The article underlines that educating not only patients but also doctors is essential to changing current prescribing practices. It is very clear that prescribing practices do need to change; there is every indication that current volumes of antibiotic usage are too high to be sustainable," Woolhouse said.
"We need to start to use antibiotics more wisely before it's too late. The longer we delay the worse the resistance problem will become."

So should you complete the course or not?
The official advice on whether or not it's essential to complete a course of antibiotics won't be likely to change immediately. Helen Stokes-Lampard, chair of the Royal College of GPs, said that while it's important that new evidence is taken on board, advice shouldn't be changed based on just one study.
"Recommended courses of antibiotics are not random. They are tailored to individual conditions and in many cases, courses are quite short – for urinary tract infections, for example, three days is often enough to cure the infection.
"We are concerned about the concept of patients stopping taking their medication mid-way through a course once they 'feel better', because improvement in symptoms does not necessarily mean the infection has been completely eradicated."
Changing the well-known message that patients should always take the full course now would "simply confuse people", she said.
"We agree with the researchers that more high quality, clinical trials are needed – and when guidelines are updated, they should take all new evidence into account. But we're not at that stage yet.
"GPs and our teams are playing a huge part in curbing the trend for overuse of antibiotics, and will prescribe in accordance with clinical guidelines, and act in the best interests of the patient in front of us – we would urge our patients not to change their behaviour based on one study."
© Copyright IBTimes 2025. All rights reserved.






















