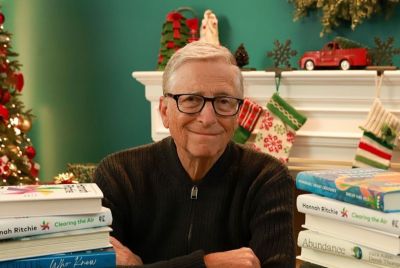
Meet Tedros Adhanom Ghebreyesus, the new Director General of the World Health Organisation
Dr Tedros served previously as health minister and foreign affairs minister in Ethiopia.

Dr Tedros Adhanom Ghebreyesus from Ethiopia, has been elected as the new Director General of the World Health Organisation. He will succeed Dr Margaret Chan.
He previously served as minister of health of Ethiopia, where he was responsible for a comprehensive health system reform. Later on, he was appointed minister of foreign affairs from 2012-2016, a position which gave him valuable diplomatic experience.
He also served as the chair on the Global Fund to Fight AIDS, Tuberculosis and Malaria board.
He talked to IBTimes UK just as he entered his final month of campaigning to become the next director general of the World Health Organisation.
WHO has often been criticised in recent years for not doing its job efficiently. Lack of funding seems to be particularly problematic. How do you plan to ensure WHO has sufficient, sustainable funding to achieve its goals?
WHO reform effort must include changes to the way the organisation is funded. Not only does it have too few resources to play the role it needs to play, as you noted, but much of its funds are also earmarked. To address WHO's funding challenges, I believe we'll need to focus on different areas.
First, focusing on value for money, so we make the most of the resources we have. Second, expanding the donor base, so WHO is not funded primarily by a small number of governments and institutions. Enhancing the flexibility of earmarked funds so WHO can invest where there are critical needs is also crucial. Finally, we need to strengthen the capacity of WHO's fundraising unit, including expanding innovative financing programmes.
Of course, all of these shifts will require us to first rebuild confidence in WHO, and to do that, we will need to be more effective and strategic in our efforts. We will have to learn to better communicate and focus on outcomes.

I will also establish an inter-ministerial advisory commission – composed of ministers of health, finance, and international development – to solicit advice, innovative solutions and recommendations on assessed financial contributions from member states. I will also engage with the highest political regional and national structures including national parliaments to
advocate on the value of WHO and investments for its cause.
The Ebola epidemic has drawn unprecedented attention to WHO's deficiencies. Do you think criticisms are justified and what would you have done differently?
The Ebola epidemic was a wake-up call. It revealed serious weaknesses in our collective capacity in emergency preparedness in a very jarring and distressing way. On the other hand, it also offered an opportunity that WHO launched serious reforms to tackle the next epidemic in a better way.
But we still have so much more we need to do.
We need to take an honest look at what we learned from Ebola and use it as an opportunity to support the development of robust health systems, particularly at the primary health care and community levels, capable of leading prevention, detection, response and recovery efforts. We need to improve local capacity to use existing resources more strategically and efficiently when public health emergencies strike.

We need to advance the full implementation of the International Health Regulations (IHR) 2005 by strengthening member states' capacity to meet and finance stipulated obligations to prevent, detect and respond to public health threats. More importantly, we need solidarity during difficult times.
As to what I would have differently, when Ebola struck, travel bans were placed on three affected countries. The bans led to serious economic consequences for these countries, and also influenced the response efforts - so I'm not sure I would have gone down that route.
Non-communicable diseases (NCDs) are the biggest killer in most countries. Is there anything that WHO can do to improve the situation?
When it comes to addressing NCDs, I believe in prevention. We need to invest in
evidence-based behaviour change strategies.
First, we need to strengthen primary health care and transfer knowledge and tips for health promotion to individuals, families, and communities. If people are informed of the risk factors and empowered with how to address them, then communities become producers of their own healthy
lifestyles. If we are going to prevent NCDs, we need individuals to be active in their own health – making healthy choices around food and physical activity among other things.
At the same time, I also believe we need to address the commercial determinants of health. For example, the overlap between food deserts and poor communities in many countries makes it impossible for some individuals to purchase healthy food and this needs to be addressed.
Finally, I also believe we need to work to support member states in their efforts to implement current resolutions on NCDs. This will require us to strengthen political leadership around NCDs and to foster multi-stakeholder engagement.

Health and climate change appear to be increasingly linked. Should WHO be concerned about climate change and what role would the organisation take under your leadership to tackle this issue?
I firmly believe that WHO should not only be concerned about climate change but it
should be a part of the solution at the front. The health impacts of climate and environmental change pose a long-term challenge to global health, including potential rises in communicable, non-communicable and vector-borne diseases.
That is why addressing the health impacts of climate and environmental change is one of
the five leadership priorities I will pursue if elected as director-general. The WHO should become a vocal advocate for mitigation strategies. It's through mitigation that we can ensure prevention.
Climate adaptation strategies are a necessary secondary component. WHO can champion global and regional coalitions which promote capacity building within countries around these strategies. It can advocate for increased financial allocations at the global, regional and national levels through
active engagement with climate financing instruments, donors and national governments.
It can work to strengthen country governments' ability to understand and use climate services and information for health policy, planning and research. And it can promote sustainability within the health sector itself, championing the use of renewable energy sources.
How likely is it that countries will achieve the sustainable development goal of universal health coverage and how can WHO help them?
I believe ensuring universal health coverage without impoverishment is the foundation for achieving the health objectives of the sustainable development goals (SDGs) – because when people are healthy, their families, communities and countries benefit.
WHO has a critical leadership role to play in making universal health coverage as the centre of gravity for the implementation of all SDGs. It has to play its role by developing new models to engage and collaborate across different stakeholders.

WHO can play a central role in compiling and disseminating best practices from countries that have achieved universal health coverage. WHO can then assist its member states in tailoring those practices to best suit its needs. Lastly, WHO can act as a catalyst to achieve UHC at national scale, including providing support for resource mobilisation.
Realising universal health coverage also needs strong commitments from and partnerships between all players, including national governments and bilateral and multilateral agencies, civil society and the private sector to overcome barriers in access to quality diagnosis and care, essential drugs and financial protection. Certainly, achieving universal health coverage will not be easy, but it is a goal we can – and must – work toward if we are to ensure everyone can live healthy, productive
lives.
Read more: How we can reform the WHO
© Copyright IBTimes 2025. All rights reserved.