AI will revolutionise the battle against cancer
Doctors and AI can work together to solve medicine's greatest challenges.
Nurse Florence Nightingale may be most well-known as the British Army's lady with the lamp, assiduously conducting night rounds and attending to the wounded by candle light. But by demonstrating the link between poor sanitary conditions and high mortality rates in hospitals, it was her pioneering use of data collection and visualisation that still resonates today.
In 2018, medicine faces a different set of challenges, with longer life expectancies and population growth increasing the number of patients suffering with chronic conditions requiring ongoing care. This has led to the cost of delivering health care increasing faster than GDP and quickly becoming unsustainable.
Transforming delivery with data
Over 160 years might have passed since Florence Nightingale's day, but addressing these challenges still depends on data. By using it to unlock valuable insights, there's an incredible opportunity to both accelerate medical breakthroughs and improve patient care.
Over the past decade, a great deal of focus has been on digitising the sector's records. But while this has been a success improving performance from an operational standpoint, we've yet to see it really transform the way we deliver services to patients. At present, health is data rich and information poor. By applying cognitive technologies like Artificial Intelligence (AI) to this data, the sector can shift from traditional reactive treatments to a more proactive health system based on prevention, wellness, faster diagnosis and precision medicine.
Nicholas McQuire, VP, Enterprise Research at analyst firm CCS Insight, sees AI "radically transform the health care industry over the next five years. AI will bring important improvements in operational effectiveness, care delivery and above all, patient outcomes. It will also be a vital tool in helping solve some of our most challenging health-related problems, not least how to balance restricted budgets and reduced workforces against the growth of chronic conditions."
Providing personalised treatment
Evolving approaches to cancer illustrate the way in which AI can revolutionise health care across the whole sector. Historically considered an acute terminal illness, medical knowledge is improving to the point where most cancers are classified as highly treatable conditions. That said, according to the World Health Organisation (WHO) between 30 and 50 percent of cancer deaths could be avoided with prevention, early detection and treatment. With the total economic impact of cancer costing the global economy over an estimated $1.16 trillion a year, we're increasingly turning to the power of AI to address this issue, with oncology one of the most advanced areas of precision medicine.
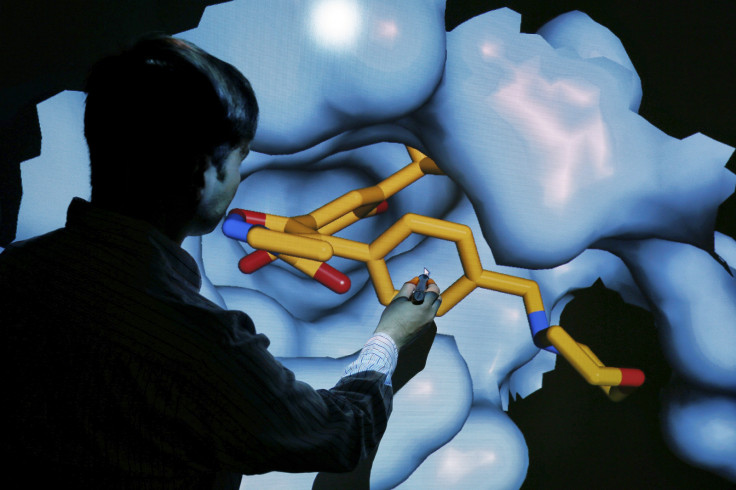
Project InnerEye, used by Addenbrooke's Hospital in Cambridge, provides a good example, applying two core branches of AI, machine learning and computer vision, for the analysis of radiological images. According to a study from TMC, the UK currently has less than five radiologists per 100,000 people, and will struggle to cope with demand for scans in the short, medium and long term. Designed to identify tumours in a matter of seconds, Project InnerEye can help speed up diagnosis, as well as improve the delivery of treatments like radiotherapy, by providing exact delineation between cancerous tissue and healthy anatomy. In addition, it promises to provide better monitoring of disease progression during treatments so they can be adjusted in line with how patients respond. This has the potential to result in more targeted and effective chemotherapy with fewer side effects for patients.
These applications provide us with an opportunity to transition from a predominantly experimental approach to the ability to be incredibly precise. Advances in genetic medicine now include genome sequencing of individual patients and tumours, allowing personalised diagnosis and treatment. While progress in this field is encouraging, due to the complex range of genetic mutations responsible for cancer, the specialist skills needed to interpret genome information, and the high volume of new cancer cases each year, it's not currently scalable to use this for every patient.
This has seen organisations like St. Jude Children's Research Hospital turn to the cloud to facilitate data sharing with global research communities. Working with Microsoft Research's genomics group, computational biologists from the hospital developed an online platform capable of managing vast quantities of anonymised genomic data. By comparing raw genomic data with reference genomes to identify where they differ, researchers hope to identify the variants responsible for cancers, and make progress toward eventually finding a cure.
Helping patients take control of their care
A key objective of these AI initiatives is minimising unnecessary and costly hospital admissions and readmissions. Discovering only eight percent of heart surgery patients were following doctor's orders upon leaving hospital, the Helsinki and Uusimaa Hospital District (HUS) wanted to tackle this issue head-on by creating a number of online 'hubs' for management of remote care plans. These range from monitoring use of medication and proscribed therapies, to providing virtual consultations with specialists.
HUS believes AI has a central role to play in optimising these kinds of virtual services. Visa Honkanen, Director of Strategic Development for HUS, explains "At the moment, we have no way of analysing what's happening, what's useful ... and how people are accessing and experiencing these services. By using machine learning to analyse the data, we will be able to direct patients to the right place right away, and also see which of our digital tools work best, abandon the tools that aren't working, and focus on the most promising ones."
Ensuring responsible use of AI
While AI presents many benefits for health care, there are important considerations that need to be taken into account. Former Director-General of the WHO Dr Margaret Chan warns "Artificial intelligence is a new frontier for the health sector... The potential of AI in health care is huge, but so is the need to take some precautions".
From a data management perspective, delivering real value with AI depends on access to a bank of patient information, a sensitive resource that needs to be safeguarded. The EU's new GDPR guidelines provide a great benchmark standard to start from, however, medical professionals, regulators and policy makers will need to address the issue of "secondary" uses for health data i.e. usage not relating to the patients direct care. Ensuring that privacy and data protections are systematically implemented will be vital for continued improvement of health care and public health. At Microsoft, we were the first major cloud provider to incorporate an international code of practice for cloud privacy, ISO/IEC 27018 and we also back those protections with strong contractual commitments.
Like Florence Nightingale founding modern nursing in 19th century, today technology and health care are collaborating to create a modern medical sector fit for the 21st. These developments will create a hybrid workforce where By helping the public play a more active, informed role in the care relationship, and empowering health professionals with the best information, AI will drive services that are more effective, efficient and accessible than ever before.
Dr. Simon Kos is Microsoft Chief Medical Officer
© Copyright IBTimes 2025. All rights reserved.