Stanford scientists identify a new subtype of depression
Scientists at Stanford Medicine have identified a new subtype of depression that affects over a quarter of patients. This new category of depression accounts for approximately 27 per cent of depressed patients.

Through the use of surveys, cognitive tests and brain imaging, scientists at Stanford Medicine in California have identified a new type of depression that affects over a quarter of patients.
This new category of depression, labelled as a cognitive biotype, accounts for approximately 27 per cent of depressed patients and can not effectively be treated by commonly prescribed antidepressants. The scientists' primary goal is to diagnose and treat the condition more precisely.
Traditionally, depression is defined as a mood disorder, so it's common practice for doctors to prescribe antidepressants that target selective serotonin reuptake inhibitors (SSRIs) in the brain.
However, this medication proves to be less effective for patients with cognitive dysfunction. The researchers believe that targeting these aforementioned dysfunctions with rarely-used antidepressants or other treatments may alleviate symptoms, whilst restoring social and occupational abilities.
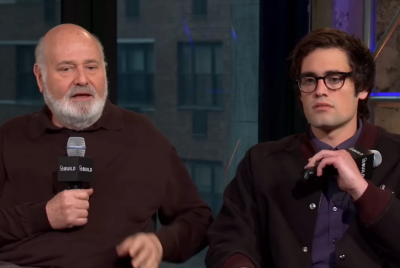
According to the study's senior author and professor of psychiatry and behavioural sciences, Leanne Williams, PhD, the published study is part of a broader effort by neuroscientists to find treatments that specifically target biotypes of depression. Professor Williams commented: "One of the big challenges is to find a new way to address what is currently a trial-and-error process so that more people can get better sooner. Bringing in these objective cognitive measures like imaging will make sure we're not using the same treatment on every patient."
For the study, 1,008 adults with major depressive disorders were randomly given one of three widely-prescribed antidepressants: escitalopram or sertraline, which both act on serotonin, or venlafaxine-XR, which acts on both serotonin and norepinephrine, with 712 participants completing the eight-week regime. Before and after treatment, the participants' depressive symptoms were measured with two surveys, one administered by a clinician, and the other being a self-assessment, which included questions relating to sleeping, eating and one's overall quality of life.
The participants later completed a series of cognitive tasks, also before and after treatment, in order to measure verbal memory, working memory, decision speed and sustained attention. Scientists used functional magnetic resonance imaging (fMRI) to scan 96 of the participants whilst they engaged in a task that involved pressing a button as quickly as possible.
The fMRI tracked neuronal activity within various brain regions by measuring changes in blood oxygen levels, with the researchers later comparing these images with individuals without depression.
Researchers discovered that 27 per cent of the participants experienced more prominent symptoms of cognitive deceleration and insomnia, impaired cognitive function and reduced activity in certain frontal brain regions, profile scientists labelled as a cognitive biotype. After treatment, the researchers also found that for the three antidepressants administered, the overall remission rates and absence of depressive symptoms greatly differed, with sertraline, for example, showing a remission rate of 35.9 per cent for those with the biotype, and 50 per cent for those without.
Laura Hack, MD, PhD, the study's lead author and assistant professor of psychiatry and behavioural studies, said: "This study is crucial because psychiatrists have few measurement tools for depression to help make treatment decisions. It's mostly making observations and self-report measures. Imaging while performing cognitive tasks is rather novel in depression treatment studies."
Both Professor Williams and Professor Hack, respectively, propose that behaviour measurement and imaging could help with diagnosing depression biotypes, leading to more effective treatment. They hope to conduct further studies on patients who have the cognitive biotype and compare different types of medication with various treatments and behavioural therapy.
© Copyright IBTimes 2025. All rights reserved.