Margareta Pagano: David Cameron, Stop NHS Political Ping Pong and Build 'National Wellness Service'
Our family doctor, Dr John Fanning, used to say he could tell what was wrong with his patients by looking into their eyes from when they walked into his surgery until they sat down on the chair next to him. On most occasions, Fanning reckoned he got the diagnosis right.
Today you are lucky if your NHS doctor bothers to look up when you walk in. Mostly, they are so glued to their computer screens that they don't often say hello, let alone take the time to look into your eyes.
There are good reasons for their bad manners, quite apart from the bad medicine; most GPs and hospital doctors are rushed, they have ten-minute slots allotted for each patient and the sheer number of people they have to see means they can't possibly know half of those they should be caring for.
But Fanning's eyes may be making a come back, in more ways than one.

In Silicon Valley, a startup bio-medical company called Augmedix has developed a secure version of Google Glass designed for doctors to wear during appointments with patients.
The glasses record video and audio allowing the doctor to consult patient records while they continue to work. Another US company, Pristine, has adapted Google Glass so surgeons wearing them can consult medical records and be hands-free while operating.
Augmedix and Pristine are just two of the many extraordinary medical devices being designed to improve healthcare in ways never dreamt of even a few years ago. Another is Proteus Digital Healthcare, which has come up with an ingestible pill carrying a chip, one made of magnesium and copper (the same as eating halibut and cashews for those who are squeamish).
Once eaten, it sends messages to a patch worn by the patient that is connected to a phone and which in turn is connected via Bluetooth to a carer or a doctor, allowing them to know whether the patient has taken his or her medication that, in some cases, could be a matter of life or death.
The chips could also keep down costs: some £7bn of the NHS' £15bn annual drugs bill is estimated to be wasted in prescription medicines either not taken or thrown away.
Power to the patients
There are masses of other examples of new devices giving power back to the patient: gadgets such as the latest Star Trek style Tricorder that monitors all bodily functions and which also connects up with a carer who is monitoring the patient; Nike arm bands measuring the number of steps you take each day; and the forthcoming Apple Watch that measures all vital signs and, of course, collects valuable data.
While these devices may appear like lifestyle, even fashion-type accessories, they have the potential to revolutionise how we approach healthcare and, if used correctly, the potential to allow for early intervention and prevention of illness and disease.

So huge is the potential that the boss of one of the NHS' biggest trusts told colleagues last week during a London gathering of health chiefs that the health institution will soon have to pay Apple a fortune for healthcare data about the public unless it invests in new technologies now.
Another NHS chief executive said his hospital was turning into a nursing home for the elderly and had done no elective work – surgery – in the last week.
All these changes, coupled with soaring life expectancy and an ageing population with multiple chronic conditions, raises fascinating challenges for the way the NHS is run. Indeed, they beg the question "what does the NHS stand for today?".
We know what the "N" means and what the "S" stands for. But what does the "H" in health mean when there is so much intelligence and information available that we have the ability to measure and improve our own health?
What role should doctors have?
Is it up to the doctors to prescribe drugs to lower cholesterol when the patient can monitor his or own levels and take their own action through diet? Should doctors prescribe drugs for patients with type 2 diabetes when the disease is caused by over eating and lack of knowledge on the part of the patient? Wouldn't it be preferable for doctors to help patients change their lifestyle, recommending nutritionists or personal trainers instead – and probably cheaper for the NHS too in the longer term?
Drug companies will have to adapt to this brave new world, too. Colm Reilly of PA Consultants says they should be accountable for the outcomes of their concoctions rather just paid on input.
He says: "We've got to stop paying for drugs on input but get the drug companies to look at outcomes and work with the health experts. But the bigger challenge is to transfer the burden of healthcare away from a centralised NHS and back to the patient."
William Beveridge, a lawyer turned economist rather than a social reformer, came up with the bones of the NHS in 1942 after being asked by the government of the day to look at ways of rebuilding Britain after the Second World War.
What Beveridge and co designed was a system of universal care to treat people with acute incidents - broken bones, infections and illnesses - whereas now most of the NHS' work is managing an ageing population with multiple chronic conditions, many of which are self-induced like diabetes or alcohol poisoning.
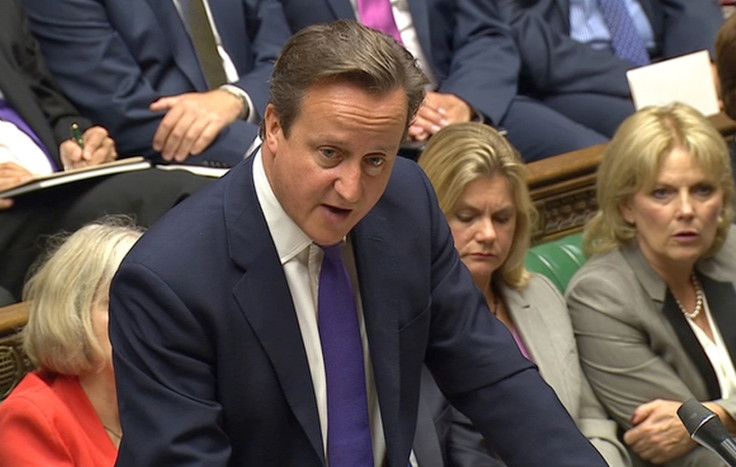
Sadly, today's politicians are too scared to make the radical commitments needed to re-imagine what the NHS should be; at present they are merely rearranging the deck chairs on the Titanic rather than re-designing it.
This is partly because of the short political lifecycle, as a thoughtful rebuilding of the NHS needs politicians who will take a 20-year view. Instead, they prefer to play political ping pong arguing about costs - which everyone knows are unsustainable - or the threat of privatisation, whereas what they should be discussing is whether we want to continue with a National Sickness Service – or invest for the long term in a NWS – a National Wellness Service.
Margareta Pagano is a business journalist who writes for the Independent and the Financial News. Follow her on Twitter @maggiepagano.
© Copyright IBTimes 2025. All rights reserved.






















