Growing up with HIV: Stigma, secrets and breakthrough
Mother to child transmission of HIV has nearly disappeared in the UK thanks to antiretroviral therapy since the AIDS epidemic started in the 1980s. Four people reveal what it's like to live with the virus.
More than 101,000 people live with HIV in the UK. Among them, children represent only a tiny and often forgotten minority.
In recent decades, improvements in the prevention and treatment of paediatric HIV have changed the face of the epidemic. Mother to child transmission of HIV has almost disappeared in the UK – the infection rate is now below 1%. Of the 860 children born to mothers living with HIV in the country during 2015, only one child acquired the virus.
Before treatments became available, being infected with HIV as a baby or as a child meant that the young patients were unlikely to make it to adulthood. This is not the case anymore. Most of those who were infected at the height of the epidemic are now young adults with a shot at living a long and healthy life.
Some of them have agreed to share their stories with IBTimes UK, to explain what it's like when the virus is something you have always known – what it's like growing up with HIV.
Despite the medical advances of recent years, these patients say they still face unique challenges and require specialist care and support. For example, it's not clear how issues such as life-long therapy, adherence to treatment, and drug resistance will impact them as they grow older. Most have experienced stigma as children and adolescents, struggling to build intimate relationships and to trust others. These experiences have left profound marks on their identity and have shaped the way they see themselves.
However, as the stigma gradually disappears, many are finding the courage to speak up and to break the taboo that surrounds HIV in children and adolescents.

"Nobody writes 'AIDS Scum' on houses anymore"
Perched on a stool in his large, luminous kitchen, Matt looks at ease as he unscrews the lid of the small bottle that contains his HIV medication. He gulps down a pill with a large glass of water.
It's been forty years since Matt was infected with the virus. Over the last decade, this daily ritual has been his lifeline, keeping him healthy and allowing him to think about the future with more serenity than he was able to before.
Matt was born with haemophilia, a genetic disorder which means his blood is not able to clot normally. The haemophilia treatment he first received as a young child was particularly invasive and uncomfortable.
However, things changed in the late 1970s, when he and other UK patients were able to receive an innovative and very effective treatment known as concentrated factor VIII, based on plasma from many different blood donors.
It was later revealed that some of these blood products were contaminated and more than 4,500 people were infected with blood-borne viruses such as HIV and hepatitis C. Matt was one of them. At the time though, no one knew what HIV was, nor that it could be passed on via blood products.
"People with bleeding disorders started injecting concentrated factor VIII. It was eventually noticed that they were starting to die from an unknown illness that had been noticed in America in gay men, and was starting to be noticed in the UK," Matt recalls.
As more and more people lost their lives to the mysterious disease, panic began to spread. In 1983, scientists finally discovered the virus at the root of the epidemic. It was given the name HTLV-III/LAV, which was later changed to HIV (human immunodeficiency virus).
The first tests for HIV were developed soon after, and doctors began testing people with haemophilia, without their knowledge. However, Matt and his family quickly heard rumours that other patients had been told they were HIV-positive. His parents tried to find out if the young boy was in the same situation, but their doctor avoided them.
"Eventually, my dad had to go the hospital, and had to physically pin my doctor against a wall to ask what was going on. That's how we found out I had been infected with the virus", Matt tells IBTimes UK.
"As a haemophiliac patient, you have an almost family relationship with your doctors. Suddenly, they were having to say to their patients 'you have been infected with this virus which in all probability will kill you, and you can't have sex.' They knew there was nothing they could do about it – and I think a lot of them struggled with that."
It was 1985 and Matt was 16 years old. He didn't entirely grasp the seriousness of the situation at first and when he did, he decided to ignore the problem as there was nothing much he could do.
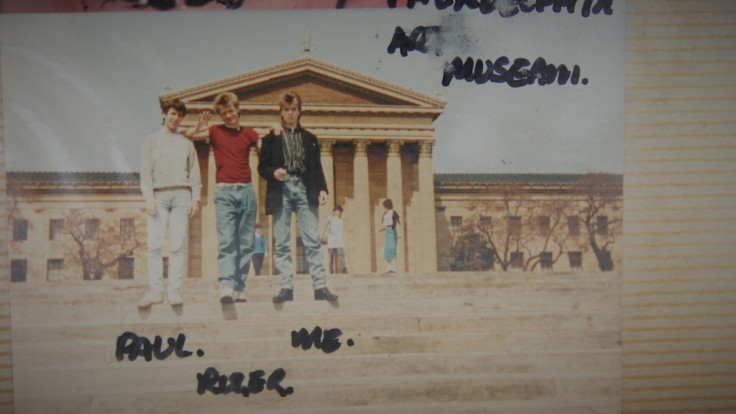
Yet his HIV diagnosis weighed on him, and had an impact on his relationships and on how he envisioned the future. Living as a teenager with HIV is challenging even for the most resilient individual today, but in the 1980s, those challenges seemed almost impossible to overcome.
Being diagnosed with HIV was seen as a death sentence, because there was no effective treatment available. AZT, the first antiretroviral drug to combat HIV, was approved by the US Food and Drugs Administration (FDA) in 1987. Patients had to face levels of stigma that are hard to imagine today.
"In the mid-80s, HIV overtook cancer as the most frightening thing in the world. People used to think that it if you shook hands or shared the same toilet seat you could get it. There were endless ways that people thought you could get HIV," Matt explains.
Matt's HIV status became his biggest secret. For years, only his family and his closest friends knew. Although he personally never had to deal with a bad reaction from anyone, he had heard enough stories of discrimination to stop him from confiding in people.
The development of effective HIV treatments in the late 80s and early 90s was a turning point for patients. For many young people like Matt, it meant they could finally dare to imagine a future life.
Matt himself didn't take the medication until 2003, when his health took a serious downturn. For years, his immune system had been able to fight off the virus on its own, but as he went through a difficult time in his professional and personal life, he suddenly became seriously ill.
Taking the medication changed a lot of things. With the treatment he takes once a day, he now has an 'undetectable' viral load. The viral load is the amount of virus present in his blood. Being undetectable doesn't mean that HIV is completely gone from the body but it does mean that people have zero chance of passing it on.
"Having treatment made it easier to tell people because it meant you could say to them 'I'm not a threat', I'm not dangerous," Matt says. And so he did. From 2009, he broke his silence and began to speak up about his status.

Today, many are still unaware that HIV-positive individuals on effective treatment cannot pass on the virus, and there are many lingering misconceptions. Despite this, people who have lived through the terrible stigma of the 80s say it's far less prevalent than it used to be.
"Nobody scribbles 'AIDS scum' on the front of your house anymore, but that used to happen. I think people have got over that, because they are not as terrified as they used to be. Having said that, it's a terrible diagnosis, it's still a terrible thing to have to deal with," Matt says.
As treatment and care given to young HIV patients continues to improve, more and more individuals infected at birth or in childhood are making it into adulthood, building relationships and living relatively normal lives.
The long term effects of the treatment are still unknown however, so it is unclear what the future holds. "I have been infected for over 40 years, and people like me are the forefront of people who have HIV; every day is a step into the unknown even on the medication we have now," Matt says.
Now, he hopes that young generations infected with HIV will be able to live long, fulfilling lives, free of discrimination. "To them I want to say, no matter what your initial reaction is, it's not the end of the world. Things have changed over the last forty years. It might take a bit of reorganising in your head and lifestyle adjustments, but take the pills, don't get stressed and just live your life."

'I was always asking the nurse why all my friends were dying'
It was the middle of winter when Becky first set foot in the UK. She was 12 years old and she was fascinated by the falling snow, which she had never seen before. This was in 2006, and Becky was travelling to be reunited with the Kroger family. They had looked after her in Cape Town when she was a baby, after her mother had died of AIDS.
This was her first time out of South Africa, where she had grown up in a home for HIV-positive children. Most of them had lost both parents to the virus. Becky herself was infected with HIV at birth, and her mother had passed away soon after. She ended up at the Kroger's house, which was registered as a 'safe place' – a home for children in distress. They cared for the infant as their own and were anguished at the thought of losing her. In a country where hundreds of children were dying from AIDS every day, and where no treatments were available to them, no one expected the little girl to live very long.
In the US, the FDA first approved the use of AZT for children in 1990. However, Becky and her friends were not able to benefit from these life-saving medicines for many years. In 1999, elements of the South African leadership embraced AIDS denialism, taking on the view that HIV does not cause AIDS and that the risks of antiretrovirals outweigh their benefits. As a result, antiretrovirals were not available for children via South Africa's public health system.
Becky was about two years old when the Krogers heard that a British charity called One to One Children's Fund was working with Cape Town's Groote Schuur hospital to conduct the first research trial in South Africa testing the use of antiretroviral drugs in children. However, for Becky to benefit, she had to go live in a Children's Home run by nuns in called Nazareth House, also located in Cape Town.

Leaving the young girl there was a heartbreaking decision for the Krogers, but it was made so that she would stand a chance of receiving treatment. Although Becky has fond memories of her years in Nazareth House, she also remembers having to deal with traumatic experiences of loss and grief. In the absence of HIV treatment, many of her friends died.
"We noticed that our friends were getting quite ill, some were dying and we had to attend a lot of funerals for them. So we were asking a lot of questions to the staff in the home, things like why did this person have to die or why do we always get sick?" Becky tells IBTimes UK.
"That's when they told us that we had a bug in our blood. At the time, they explained very simple things, and told us that there was no medicine for it, but that they were doing everything they could to make sure that we were happy."
Becky's own health was often quite poor, and she suffered a lot from eye and ear infections and stomach bugs. "I just thought that was normal at the time. I didn't think that I could actually be as healthy as I am today," she says.
In 2003, the One to One Children's Fund piloted the first antiretroviral trial for children in Cape Town, and Becky was one of the first children selected to participate.

She vividly remembers the syringes full of liquids that she was given. She remembers the bad taste that these treatments left in her mouth and the stomach pains it gave her. She suffered from serious side effects from the first medicines she received, and even had to be hospitalised. She remained sick and very frail, until the doctors eventually figured out which drugs were having these effects. She was given another drug regimen, and slowly, her health improved.
"One day I decided I didn't want to be in hospital anymore and I let my doctor know that. He said 'you know what, that's the best thing a child has ever said to me,' because it meant to him that I was strong enough to leave the hospital, to run around and to eat as much food as I really wanted to, when I didn't really have an appetite before," Becky says.
Taking the medicine on time every day is key to remaining healthy and to bring the viral load – the amount of virus present in the blood – to undetectable levels. For Becky, it has never really been an issue in her childhood, as she took them with the other children at Nazareth House. She didn't feel like she was different from everyone else.
Adhering to treatment can be a significant challenge for children. "The aim of treatment is to get the viral load to undetectable levels and to let the immune system function as it should. For this, we have to get children to take their medication every day and to understand why they are taking it every day. That's one of the big challenges, explaining to a child what is wrong with them, that's quite tough," Dr Jennifer Evans, Consultant Paediatrician at the Noah's Ark Children's Hospital for Wales, tells IBTimes UK.
The role of family environment is crucial to make sure that children and adolescents do take the medicine. It is unrealistic to think that adolescents will assume responsibility for medication given what goes on in their lives – from peer pressure to chaotic social schedules and issues relating to stigma and body image. Forgetting to follow the treatment – or stopping it altogether – not only puts young people at risk of seeing their viral load jump back up and their disease progress, but it also increases the risk of HIV drug resistance.
After Becky's first visit to the UK in 2006, the Kroger family decided to adopt her. Spending her adolescence in England, Becky discovered that her HIV status did set her apart from her peers. Each time the alarm on her phone rang, telling her to take her pills, it was a reminder of her difference. She realised that following this routine could at times be difficult.
Despite this, Becky has never been tempted to discontinue her treatment. She knows that HIV medication save lives, and it has saved hers. From a child who was not expected to live very long, she has become a healthy young woman pursuing her dream of working in a school.

'Knowing that my son is healthy and happy is such a relief'
One-year-old Kyle is squealing with delight as he turns the wheel of his miniature car in the middle of the living room. Sitting quietly on the sofa, his mother Paida looks on proudly.
Paida was seven years old when she left her native Zimbabwe to move to Rochdale, a small town not far from Manchester. Over the last 14 years, she has made a home for herself there, and now for her young son as well.
But she has not always been this happy in Rochdale. She was about to begin secondary school when she learned she was HIV-positive. Paida was infected at birth, as her mother had not been aware of her own status.
Throughout her teenage years, this diagnosis weighed heavily on her. "Where I grew up, HIV is something that was considered really bad. It was the thing you wouldn't want one of your family members to have. Where I grew up, if you had HIV, nobody wanted you near their loved ones. Just knowing that HIV was something you should not have, it really affected me," Paida says.

Her relationships with her friends and family reached an all-time low after that. Convinced that she was going to die, she began acting out in school and became indifferent to people around her.
"I would do everything I could to get kicked out of school, I just didn't care anymore. I just didn't care about anyone. I kept being naughty so that I wouldn't have to be near the other kids. I felt alone and thought 'do I tell someone?' I was at school keeping this huge secret and I was just really paranoid," Paida explains.
It wasn't until she joined the children's charity Barnardo's, that she learned more about HIV and realised she wasn't about to die anytime soon. It gave her courage to eventually disclose her status. The stigma she experienced was as bad as she had dreaded. The other pupils in her school made fun of her and some of their parents complained, saying that she should not be able to attend the same classes.
"I also remember when I got my first job, in a restaurant. Someone actually put a Facebook status asking why I was allowed to work with food when I was HIV-positive. They thought I could easily infect other people just by preparing the food. It just didn't make sense," Paida recalls.
Facing these hurtful remarks was hard, but perhaps most difficult was dealing with one of her greatest fears – that she would never be able to have children. HIV can be passed on from an HIV-positive mother to her children during pregnancy, labour, delivery or breastfeeding. Studies have shown that in the absence of intervention, transmission rates range from 15 to 45%. Prior to the development of antiretroviral medication, thousands of babies around the world were infected in this way.
In recent years, appropriate treatment and care for HIV-positive women has reduced this risk significantly. It is estimated that in the last two decades, 1.6 million new HIV infections among children have been averted. In some countries, such as the UK where Paida gave birth to Kyle, infection rates for babies born to HIV-positive mothers are now extremely low.
"Now with interventions and careful monitoring during pregnancy you can get it to below 1%," Dr Jennifer Evans, Consultant Paediatrician at the Noah's Ark Children's Hospital for Wales tells IBTimes UK. "So mother-to-child transmission is not 100% preventable but it's much more controllable."
Paida's viral load was already undetectable when she found out she was pregnant, thanks to the treatments she had been taking daily since childhood. She continued taking those treatments throughout her pregnancy, substantially lowering the risk of infecting her baby.

Kyle was tested at birth and when he was six months old. Both tests suggested that he is HIV-negative. Paida says he will get one last test at the age of two.
She has not breastfed him, to avoid passing on the virus through her milk. This has not been a problem for her, but for many women this is one of the most complicated aspects of being a young mother with HIV.
"Because HIV can be passed on through breast milk we tend to give the mums drugs to stop their breast milk and they bottle feed to reduce the chances of babies acquiring HIV," explained Dr Jake Bayley, Trustee of charity Terrence Higgins Trust and Sexual Health Consultant at Barts NHS Trust.
"For some women, especially in the African community, it can be hard. If you don't breastfeed, people will think you have HIV. We sometimes have had to construct stories for them to tell, like they've got problem with their milk or mastitis, so the people don't realise that they're living with HIV."
Paida now looks to the future with much more optimism. When her son grows up, she won't be scared of telling him about her status.
"Having a child is something that I've always wanted, but I was really scared for Kyle. Just knowing that he is healthy, that he is HIV-negative and has never been in hospital, that's just a relief. In the future, I would love for him to have more siblings. And I know he'll be a sign of hope, as he'll be able to tell people that he was born to an HIV-positive mother, but was not infected."

'As Miss Congo UK, I speak up about my status'
"When the nurse told me I was HIV-positive, I stood completely still. I was devastated. Growing up in the Congolese community and watching Congolese films as a child, I knew that for people around me, HIV meant AIDS, it meant I was going to die," Horcelie says.
With her long blue dress and her sophisticated golden make-up which makes her look older than her 22 years, you'd have no trouble believing that Horcelie just won a beauty pageant.
In April 2017, the young woman was crowned Miss Congo UK, after a long and emotional competition. Her win has been life-changing, giving her a very public platform to raise awareness about HIV. Around the same time, Horcelie decided to disclose her status to all her loved-ones.
Ever since learning that she was HIV-positive as a little girl, Horcelie had kept this a secret even from her closest friends. Until last year, most had no idea that she was living with the virus.
"I never told anyone, not when I was a teenager. I was struggling to find myself. So many things are happening around you when you are around that age and HIV was the biggest one. I use to tell myself 'how do I go and tell someone?"
She feared people's reaction, particularly after growing up in a community that deeply stigmatised its HIV-positive members and that considered sex a taboo.
"There's a lot of stigma attached to women who are HIV-positive. People say they have been sleeping around. In a sense, I'm lucky because I told people when I was still quite young. If I had been in my thirties, people would have assumed that I had been dating, that I had been with men. There would be a complete dismissal of the fact I was born HIV-positive," Horcelie explains.
Since no one knew about her status, no one ever said anything hurtful to her when she was a teenager. But Horcelie remembers hearing some of her friends in high school gossip about HIV-positive people and saying they would never date someone who had been infected. These comments, exchanged without malice in the playground, really brought her spirit down.

The stigma and cultural taboos that Horcelie encountered growing up sometimes soured her relationship with her parents. She resented her diagnosis, resented the fact that they had passed on a virus that could make her a pariah in her community.
"For me it was a judgement upon my parents, and I didn't know how to begin to forgive them. There were times when things became a bit quiet between us. I didn't know how to confront my mother, and start a conversation about it. It was very difficult but as I grew up I learned to recognise that people make mistakes that hurt others. I have to remember that my parents, what they did was not intentional. I have now learned to forgive. It was definitely a journey," Horcelie says.
Living with the virus also made Horcelie wary of engaging in any serious relationships with men. The ones she did date often struggled to accept her as an HIV-positive woman. "The ignorance is large especially with men. If you are a woman and you are HIV-positive the men just dismiss it, they don't care, they say 'you have been sleeping around, I don't want to date someone like that, I don't want people to know.' One of my boyfriends wanted it to be a secret for us two. He feared other people's judgement," Horcelie adds.
"But the more it was becoming a secret, the more it was hurting me. It brought me down a lot, I didn't feel like I was a human being. But this kind of behaviour is not just hurting me, it is hurting people who are not so lucky as to be on treatment, and may think 'how do I go on dating?'"

Horcelie is now determined to use her voice as Miss Congo UK to change people's perception of HIV-positive women, especially in the African community. She won't be with a man, unless he can respect the important work she is doing and recognise the importance of sharing her story publicly.
Speaking up is not just liberating for her, helping her to come to terms with her status; it is above all a way to give a voice to the millions of women infected with HIV worldwide, who are silenced everyday by taboo, discrimination and fear.
HIV vs AIDS:HIV and AIDS are not the same thing. HIV stands for human immunodeficiency virus. It is found in the body fluids of an infected person including semen, vaginal and anal fluids, blood, and breast milk. HIV targets the immune system.It is a virus that cannot grow or reproduce on its own. To make new copies of itself, it has to infect immune system cells known as CD4 cells. This damages the immune system and gradually weakens people's natural defences - leaving them vulnerable to infections.
Without treatment, HIV leads to acquired immunodeficiency syndrome, or AIDS - the most severe phase of HIV infection. The immune system of people with AIDS is so damaged that it can't fight off severe infections and illnesses.
With an early diagnosis and effective treatments however, most people with HIV do not develop any AIDS-related illnesses, live a near-normal lifespan and can't pass on the virus to anyone else.
HIV-positive: Being HIV-positive means a patient has tested positive for the virus and that HIV is present in the blood stream.
CD4 cells: CD4 cells are white blood cells that are targeted by HIV. They play an important role in the immune system. The CD4 cell count - the number of blood cells in a cubic millimetre of blood - can give a good indication of the health of a person's immune system.
Viral load: The level of HIV in a person's bloodstream.
Undetectable: When people take their HIV drugs every day as prescribed, this prevents the virus from making copies of itself. When this happens, the amount of HIV in a person's blood stream goes down to a level so low it cannot be detected - the person's viral load is 'undetectable'. Studies have shown that people on effective treatment who are undetectable have a zero chance of transmitting the virus.
Antiretrovirals: Unlike some other viruses, the human body can't get rid of HIV completely, so once you get HIV, you have it for life. There is no cure or vaccine at present. However, the advent of antiretroviral therapy has allowed people to live long and healthy lives and to reduce the risk of transmitting the virus to zero. Antiretroviral therapy consists of the combination of antiretroviral (ARV) drugs that stop the HIV virus from replicating and stop the progression of HIV condition.
HIV transmission: HIV is spread mainly through sexual contact or sharing drug injection equipment, such as needles, with someone who has HIV. Mother to child transmission at birth or through breastmilk is possible, but many steps in recent decades have been taken to reduce this risk dramatically.
© Copyright IBTimes 2025. All rights reserved.